PLN mentioned in article about inadequate medical care by CMS at GA jail
Augusta Chronicle, Jan. 1, 2009.
http://chronicle.augusta.com/stories/2009/08/30...
PLN mentioned in article about inadequate medical care by CMS at GA jail - Augusta Chronicle 2009
Deaths in jails raise questions about care
By Sandy Hodson | Staff Writer - Augusta Chronicle
Sunday, August 30, 2009
Since the decade began, at least nine men have died while in the custody of the Richmond County jail. Officially, they were not guilty of anything, but they were being held until the justice system could determine whether charges against them could be proven.
Those who died varied from a troubled Vietnam vet to a brain-damaged traffic victim with the mental capacity of a child. Another was a mentally ill inmate who should have been a free man, but the paperwork releasing him never made it to the jail.
All the deaths were investigated. No criminal wrongdoing was found.
The Augusta Chronicle reviewed the cases at the urging of families and others who all seemed to want the answer to one simple question: How could someone in the restrictive and rigidly supervised custody of incarceration end up dead?
IN A PLACE WHERE slaying suspects and tough-talking young men live behind steel doors and iron bars, the old, handicapped, depressed or mentally ill can be overlooked.
Charles Brunson was severely disabled when he died at the jail March 12, 2008. The only public notice of his death was an obituary. The severely disabled and brain damaged 52-year-old might have never been thought of again by anyone outside his family, except that he suffered a fatal head injury inside the county jail at 401 Walton Way. Less than four years earlier, another inmate suffered a near-fatal head injury that an emergency room doctor said was exacerbated because of a delay in treatment.
Like most people housed in the Richmond County jail, Mr. Brunson had been arrested but not convicted. The Chronicle learned of Mr. Brunson while reviewing the quality of medical care at the jail facilities because of two recent lawsuits involving former inmates and a steady stream of complaints sent to the newspaper by phone, e-mail, and letters written in pencil by inmates.
Since 2003, Augusta has contracted with Correctional Medical Services to provide medical services in the county jails. This year's contract is worth more than $4 million. CMS, the largest U.S. corporation in the prison health care business, takes care of all medical needs, from nurses and doctors to medicine and equipment.
Maj. Gene Johnson, who is in charge of the jails on Walton Way and Phinizy Road, said he believes the inmates have better health care than most county residents. Every day he meets with the registered nurse in charge of medical services to discuss any especially troubling medical problems among nearly 1,000 inmates, most of whom Maj. Johnson knows by name or accused deed.
"They're getting better care here than they can on the street," Maj. Johnson said.
Some are getting care for the first time in years. Many have abused themselves for years with drugs and alcohol at a higher level than the general population, he said.
The $17.7 million budget for the jails includes just more than $5.1 million for medical care. In addition to the contract payment to CMS, the city is liable for any medical expenses that exceed $10,000 for any single inmate in a single year.
CMS spokesman Ken Fields said the company provides qualified and experienced health care professionals to see to the medical needs of the jail inmates. That quality is recognized in the jail's accreditation by the National Commission on Correctional Healthcare, he said.
THE ACCREDITATION, however, doesn't impress everyone.
Attorney Elizabeth Alexander, the director of the American Civil Liberties Union's national prison project, said that means the facility can provide an adequate level of care. The way CMS and other for-profit corporations in the business of prison health care make money is the problem, she said. The companies get contracts by providing the lowest bid, and the only place to cut costs is in the medical care, said Ms. Alexander, who works from the ACLU's New York City office..
Once the contracts are set, there's no oversight of the care because the state or local officials no longer have independent medical staff, she said.
Ms. Alexander represented the family of 21-year-old Timothy Joe Souders in its lawsuit against the state of Michigan and CMS. Mr. Souders, who was mentally ill, was chained to a bed for 17 hours a day for four days in a cell that got as hot as 106 degrees, according to court documents. He died of dehydration. A surveillance video showed Mr. Souders' experience, and the state agreed to a $3.8 million settlement in June 2008.
"We're quite familiar with CMS," Ms. Alexander said. The company has a long history of providing inadequate and often unconstitutional care, she said.
It's not the only poor-performing prison health care company, she said. States and local governments go from one to the other and back again, usually with the same results, she said. The only real solution she sees is to use nonprofit-based medical personnel.
Mr. Fields pointed to CMS' 30 years of experience in what is a speciality in the medical industry. CMS has been a leader in the field, he said, and has developed strategies and techniques that have improved the quality of care in secured facilities.
CMS has been named in many lawsuits, but numbers don't equate to a lack of quality care, Mr. Fields said. He estimated that 95 percent of the suits are dismissed or won by CMS.
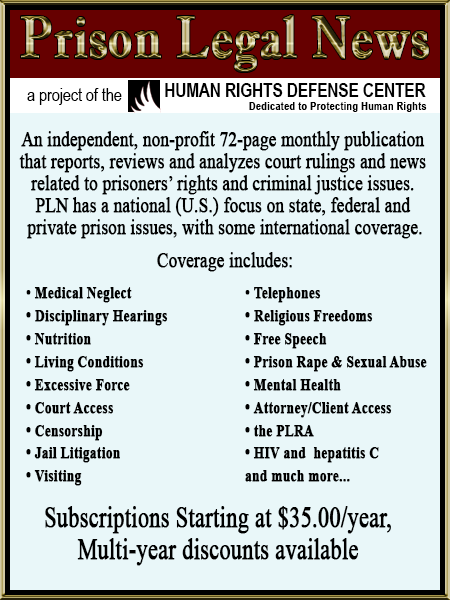
The Chronicle searched for lawsuits involving CMS by using legal databases maintained by Justia.com, a private company that provides free access to courts and other legal issues, and Prison Legal News, a prisoner rights advocacy organization.
The Chronicle found 182 lawsuits against CMS. State and local governments who have contracted with CMS have had to pay settlements in 16 cases that totaled more than $28.5 million.
Still, CMS wins almost all of the cases, and the same is true of state and local governments sued by inmates who complained about the quality of health care.
IN FEDERAL COURT IN AUGUSTA, inmates have sued the county 31 times in the past decade. Nineteen suits alleged civil rights violations based on medical services. The city won every case. Another lawsuit, filed by the mother of a man who died of untreated pneumonia, is pending.
In most of those lawsuits, the county didn't even have to respond to the allegations, thanks to federal legislation passed in 1995. The Prison Litigation Reform Act was designed to curb the flood of prisoner lawsuits in federal court. It allows judges to summarily toss out what they see as frivolous cases.
Ms. Alexander said the law and case decisions have set the bar at a near impossible height, regardless of the merit of an inmate's complaint. An inmate can't claim a constitutional violation based on health care unless he suffered physical harm, Ms. Alexander said. An inmate also has to prove the staff knew harm could happen but did nothing to prevent it, she said.
The techniques once used at the Abu Ghraib prison in Iraq wouldn't be considered civil rights violations in the U.S. legal system, Ms. Alexander said. The inmates didn't suffer actual physical harm.
In an opinion released in January 2007, Supreme Court Chief Justice John Roberts wrote that trial judges and appellate courts were taking the Prison Litigation Reform Act too far.
"We are not insensitive to the challenges faced by the lower federal courts in managing their dockets and attempting to separate, when it comes to prisoner lawsuits, not so much wheat from chaff as needles from haystacks. However ... adopting different and more onerous pleading rules" is not right, he wrote.
Jamie Koss is among those whose constitutional claim based on health care was tossed out in the Augusta federal court.
He suffered a head injury in the Richmond County jail Dec. 1, 2004. As he lay unconscious on the cement floor, a nurse did little more than glance at Mr. Koss before deciding he was fine, according to witness statements in the GBI file on Mr. Koss' injury, according to his lawsuit. About seven hours passed before Mr. Koss got help. The delay, the treating physician at University Hospital said, exacerbated the brain damage. He is now disabled, in chronic pain and unable to care for himself, according to his lawsuit.
Mr. Koss might have had a case against the nurse who did nothing to help him, but because she has died, Mr. Koss had no valid constitutional challenge, the judge ruled. Neither the sheriff's office nor CMS can be held liable for the nurse's derogation of duty.
Mr. Koss, the judge ruled, could not meet the legal standard for such a constitutional challenge: that CMS or the sheriff's office participated in the acts or omissions; that either had a history of widespread abuse so that they should have known there was a risk; or either implemented a policy that resulted in deliberate indifference.
When asked about Mr. Koss' case, Mr. Fields said CMS cannot discuss any patient's care because of confidentiality demanded of health care professionals.
After death, federal medical privacy laws allow the release of a person's medical information only to the executor of the estate; the person authorized access through a health care power of attorney immediately before death; or a person authorized by the patient while still alive to receive the information, wrote Christine Shaffer, an Augusta attorney with experience in litigation dealing with the privacy law and the state's Open Records Act.
Maj. Johnson said the Richmond County jail staff is doing its best to keep watch over the inmates in the overcrowded facilities and separate those who are vulnerable or ill.
"This jail here has turned into a mental institution," he said one particularly trying morning in June. Georgia Regional Hospital was full and not accepting new patients, Maj. Johnson said, and he had one out-of-control inmate who broke the iron-restraint chair and tore the ligaments in a captain's thumb.
THERE ARE PROCEDURES SET to catch potential medical problems on the front end, Maj. Johnson said.
Every person brought into the jail is asked a set of questions to determine whether he or she has any medical needs or could be suicidal. A nurse is to check the answers and follow up on any potential medical needs.
Every person can fill out a request to see the CMS physician or dentist, Maj. Johnson said, but the requests are screened by a nurse to determine whether an inmate should see the doctor. The doctor works 40 hours a week.
On any given day, the jail facilities hold a combined population of about 1,000. A recent article in a John Hopkins University publication found the average ratio of physician to patients in the United States is 1 to 400.
What medicine an inmate receives is up to the physician, Maj. Johnson said. Jail staff cannot allow family or anyone else to provide medication for an inmate because staffers have no way to verify what it is, he said.
In lawsuits, former inmates have complained that they cannot get access to the nurses and especially to the doctor.
Maj. Johnson denies those charges. Inmates have access to medical care, and the medical staff is trained to deal with inmates incapable of asking for medical attention, he said. Dealing with mentally ill inmates is a huge issue for the medical and jail staffs, he said.
There have been at least five suicides since 2001. According to GBI reports reviewed by The Chronicle , most had been on antidepressants.
John O. Johnson was a 43-year-old repeat offender looking at life in prison if convicted of a series of armed robberies. After his May 21, 2003, arrest, he tried to choke himself to death with a shoestring and he banged his head into a wall. The jail put him on suicide watch.
Mr. Johnson convinced the medical staff he was all right, according to the GBI report. He was moved to the special needs unit in a lock-down status, but he was allowed to have clothing and the normal items other inmates have. The morning after he was moved off suicide watch, Mr. Johnson was found hanging from a strip of bedsheet.
He left handwritten copies of a will and testament and letters of apology to his mother and the mother of his children. He also left a note apologizing to the people of Richmond County for his crimes.
According to a statement given by one of the nurses, Mr. Johnson swore he would kill himself because staff couldn't watch him all of the time.
though not many people have died in the county jails in recent years, the number shouldn't be the criterion for judging the quality of medical care, said Ms. Alexander, who has been with the ACLU Prison Project since 1981.
The critical question is whether any of the deaths were preventable, Ms. Alexander said. The only way to know for sure is to examine the medical records, she said.
If something went wrong, the problem needs to be understood and corrected, she said. She compared it to how the National Transportation Safety Board operates. Compared with the number of flights every year, the number of crashes is not statistically significant, but the board examines every accident to find out what happened and whether there was a problem that can be corrected to prevent another accident, she said.
Though Mr. Koss' near-fatal head injury in December 2004 was exacerbated because of a delay in treatment, when Mr. Brunson struck his head in March 2008, the nurse took no action to determine whether the severely disabled and brain-damaged man might have had a brain injury, according to the GBI file.
Mr. Brunson's family isn't seeking civil unrest or damages from lawsuits. They say they just wanted to know why he couldn't have been saved.
Reach Sandy Hodson at (706) 823-3226 or sandy.hodson@augustachronicle.com
Deaths in jails raise questions about care
By Sandy Hodson | Staff Writer - Augusta Chronicle
Sunday, August 30, 2009
Since the decade began, at least nine men have died while in the custody of the Richmond County jail. Officially, they were not guilty of anything, but they were being held until the justice system could determine whether charges against them could be proven.
Those who died varied from a troubled Vietnam vet to a brain-damaged traffic victim with the mental capacity of a child. Another was a mentally ill inmate who should have been a free man, but the paperwork releasing him never made it to the jail.
All the deaths were investigated. No criminal wrongdoing was found.
The Augusta Chronicle reviewed the cases at the urging of families and others who all seemed to want the answer to one simple question: How could someone in the restrictive and rigidly supervised custody of incarceration end up dead?
IN A PLACE WHERE slaying suspects and tough-talking young men live behind steel doors and iron bars, the old, handicapped, depressed or mentally ill can be overlooked.
Charles Brunson was severely disabled when he died at the jail March 12, 2008. The only public notice of his death was an obituary. The severely disabled and brain damaged 52-year-old might have never been thought of again by anyone outside his family, except that he suffered a fatal head injury inside the county jail at 401 Walton Way. Less than four years earlier, another inmate suffered a near-fatal head injury that an emergency room doctor said was exacerbated because of a delay in treatment.
Like most people housed in the Richmond County jail, Mr. Brunson had been arrested but not convicted. The Chronicle learned of Mr. Brunson while reviewing the quality of medical care at the jail facilities because of two recent lawsuits involving former inmates and a steady stream of complaints sent to the newspaper by phone, e-mail, and letters written in pencil by inmates.
Since 2003, Augusta has contracted with Correctional Medical Services to provide medical services in the county jails. This year's contract is worth more than $4 million. CMS, the largest U.S. corporation in the prison health care business, takes care of all medical needs, from nurses and doctors to medicine and equipment.
Maj. Gene Johnson, who is in charge of the jails on Walton Way and Phinizy Road, said he believes the inmates have better health care than most county residents. Every day he meets with the registered nurse in charge of medical services to discuss any especially troubling medical problems among nearly 1,000 inmates, most of whom Maj. Johnson knows by name or accused deed.
"They're getting better care here than they can on the street," Maj. Johnson said.
Some are getting care for the first time in years. Many have abused themselves for years with drugs and alcohol at a higher level than the general population, he said.
The $17.7 million budget for the jails includes just more than $5.1 million for medical care. In addition to the contract payment to CMS, the city is liable for any medical expenses that exceed $10,000 for any single inmate in a single year.
CMS spokesman Ken Fields said the company provides qualified and experienced health care professionals to see to the medical needs of the jail inmates. That quality is recognized in the jail's accreditation by the National Commission on Correctional Healthcare, he said.
THE ACCREDITATION, however, doesn't impress everyone.
Attorney Elizabeth Alexander, the director of the American Civil Liberties Union's national prison project, said that means the facility can provide an adequate level of care. The way CMS and other for-profit corporations in the business of prison health care make money is the problem, she said. The companies get contracts by providing the lowest bid, and the only place to cut costs is in the medical care, said Ms. Alexander, who works from the ACLU's New York City office..
Once the contracts are set, there's no oversight of the care because the state or local officials no longer have independent medical staff, she said.
Ms. Alexander represented the family of 21-year-old Timothy Joe Souders in its lawsuit against the state of Michigan and CMS. Mr. Souders, who was mentally ill, was chained to a bed for 17 hours a day for four days in a cell that got as hot as 106 degrees, according to court documents. He died of dehydration. A surveillance video showed Mr. Souders' experience, and the state agreed to a $3.8 million settlement in June 2008.
"We're quite familiar with CMS," Ms. Alexander said. The company has a long history of providing inadequate and often unconstitutional care, she said.
It's not the only poor-performing prison health care company, she said. States and local governments go from one to the other and back again, usually with the same results, she said. The only real solution she sees is to use nonprofit-based medical personnel.
Mr. Fields pointed to CMS' 30 years of experience in what is a speciality in the medical industry. CMS has been a leader in the field, he said, and has developed strategies and techniques that have improved the quality of care in secured facilities.
CMS has been named in many lawsuits, but numbers don't equate to a lack of quality care, Mr. Fields said. He estimated that 95 percent of the suits are dismissed or won by CMS.
The Chronicle searched for lawsuits involving CMS by using legal databases maintained by Justia.com, a private company that provides free access to courts and other legal issues, and Prison Legal News, a prisoner rights advocacy organization.
The Chronicle found 182 lawsuits against CMS. State and local governments who have contracted with CMS have had to pay settlements in 16 cases that totaled more than $28.5 million.
Still, CMS wins almost all of the cases, and the same is true of state and local governments sued by inmates who complained about the quality of health care.
IN FEDERAL COURT IN AUGUSTA, inmates have sued the county 31 times in the past decade. Nineteen suits alleged civil rights violations based on medical services. The city won every case. Another lawsuit, filed by the mother of a man who died of untreated pneumonia, is pending.
In most of those lawsuits, the county didn't even have to respond to the allegations, thanks to federal legislation passed in 1995. The Prison Litigation Reform Act was designed to curb the flood of prisoner lawsuits in federal court. It allows judges to summarily toss out what they see as frivolous cases.
Ms. Alexander said the law and case decisions have set the bar at a near impossible height, regardless of the merit of an inmate's complaint. An inmate can't claim a constitutional violation based on health care unless he suffered physical harm, Ms. Alexander said. An inmate also has to prove the staff knew harm could happen but did nothing to prevent it, she said.
The techniques once used at the Abu Ghraib prison in Iraq wouldn't be considered civil rights violations in the U.S. legal system, Ms. Alexander said. The inmates didn't suffer actual physical harm.
In an opinion released in January 2007, Supreme Court Chief Justice John Roberts wrote that trial judges and appellate courts were taking the Prison Litigation Reform Act too far.
"We are not insensitive to the challenges faced by the lower federal courts in managing their dockets and attempting to separate, when it comes to prisoner lawsuits, not so much wheat from chaff as needles from haystacks. However ... adopting different and more onerous pleading rules" is not right, he wrote.
Jamie Koss is among those whose constitutional claim based on health care was tossed out in the Augusta federal court.
He suffered a head injury in the Richmond County jail Dec. 1, 2004. As he lay unconscious on the cement floor, a nurse did little more than glance at Mr. Koss before deciding he was fine, according to witness statements in the GBI file on Mr. Koss' injury, according to his lawsuit. About seven hours passed before Mr. Koss got help. The delay, the treating physician at University Hospital said, exacerbated the brain damage. He is now disabled, in chronic pain and unable to care for himself, according to his lawsuit.
Mr. Koss might have had a case against the nurse who did nothing to help him, but because she has died, Mr. Koss had no valid constitutional challenge, the judge ruled. Neither the sheriff's office nor CMS can be held liable for the nurse's derogation of duty.
Mr. Koss, the judge ruled, could not meet the legal standard for such a constitutional challenge: that CMS or the sheriff's office participated in the acts or omissions; that either had a history of widespread abuse so that they should have known there was a risk; or either implemented a policy that resulted in deliberate indifference.
When asked about Mr. Koss' case, Mr. Fields said CMS cannot discuss any patient's care because of confidentiality demanded of health care professionals.
After death, federal medical privacy laws allow the release of a person's medical information only to the executor of the estate; the person authorized access through a health care power of attorney immediately before death; or a person authorized by the patient while still alive to receive the information, wrote Christine Shaffer, an Augusta attorney with experience in litigation dealing with the privacy law and the state's Open Records Act.
Maj. Johnson said the Richmond County jail staff is doing its best to keep watch over the inmates in the overcrowded facilities and separate those who are vulnerable or ill.
"This jail here has turned into a mental institution," he said one particularly trying morning in June. Georgia Regional Hospital was full and not accepting new patients, Maj. Johnson said, and he had one out-of-control inmate who broke the iron-restraint chair and tore the ligaments in a captain's thumb.
THERE ARE PROCEDURES SET to catch potential medical problems on the front end, Maj. Johnson said.
Every person brought into the jail is asked a set of questions to determine whether he or she has any medical needs or could be suicidal. A nurse is to check the answers and follow up on any potential medical needs.
Every person can fill out a request to see the CMS physician or dentist, Maj. Johnson said, but the requests are screened by a nurse to determine whether an inmate should see the doctor. The doctor works 40 hours a week.
On any given day, the jail facilities hold a combined population of about 1,000. A recent article in a John Hopkins University publication found the average ratio of physician to patients in the United States is 1 to 400.
What medicine an inmate receives is up to the physician, Maj. Johnson said. Jail staff cannot allow family or anyone else to provide medication for an inmate because staffers have no way to verify what it is, he said.
In lawsuits, former inmates have complained that they cannot get access to the nurses and especially to the doctor.
Maj. Johnson denies those charges. Inmates have access to medical care, and the medical staff is trained to deal with inmates incapable of asking for medical attention, he said. Dealing with mentally ill inmates is a huge issue for the medical and jail staffs, he said.
There have been at least five suicides since 2001. According to GBI reports reviewed by The Chronicle , most had been on antidepressants.
John O. Johnson was a 43-year-old repeat offender looking at life in prison if convicted of a series of armed robberies. After his May 21, 2003, arrest, he tried to choke himself to death with a shoestring and he banged his head into a wall. The jail put him on suicide watch.
Mr. Johnson convinced the medical staff he was all right, according to the GBI report. He was moved to the special needs unit in a lock-down status, but he was allowed to have clothing and the normal items other inmates have. The morning after he was moved off suicide watch, Mr. Johnson was found hanging from a strip of bedsheet.
He left handwritten copies of a will and testament and letters of apology to his mother and the mother of his children. He also left a note apologizing to the people of Richmond County for his crimes.
According to a statement given by one of the nurses, Mr. Johnson swore he would kill himself because staff couldn't watch him all of the time.
though not many people have died in the county jails in recent years, the number shouldn't be the criterion for judging the quality of medical care, said Ms. Alexander, who has been with the ACLU Prison Project since 1981.
The critical question is whether any of the deaths were preventable, Ms. Alexander said. The only way to know for sure is to examine the medical records, she said.
If something went wrong, the problem needs to be understood and corrected, she said. She compared it to how the National Transportation Safety Board operates. Compared with the number of flights every year, the number of crashes is not statistically significant, but the board examines every accident to find out what happened and whether there was a problem that can be corrected to prevent another accident, she said.
Though Mr. Koss' near-fatal head injury in December 2004 was exacerbated because of a delay in treatment, when Mr. Brunson struck his head in March 2008, the nurse took no action to determine whether the severely disabled and brain-damaged man might have had a brain injury, according to the GBI file.
Mr. Brunson's family isn't seeking civil unrest or damages from lawsuits. They say they just wanted to know why he couldn't have been saved.
Reach Sandy Hodson at (706) 823-3226 or sandy.hodson@augustachronicle.com