Amfar Issue Brief-hiv in Correctional Settings March 2008
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
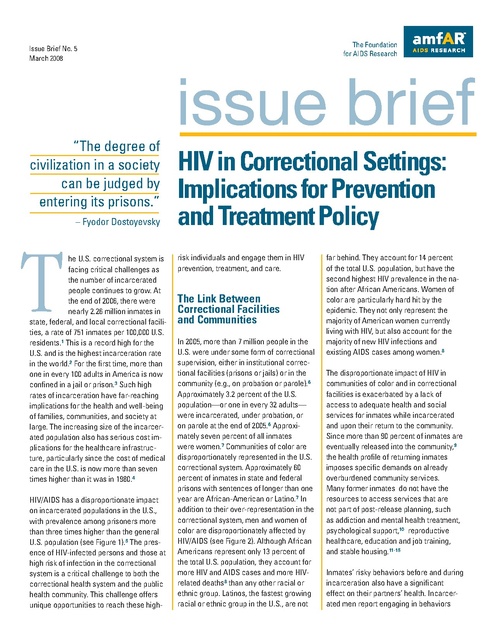
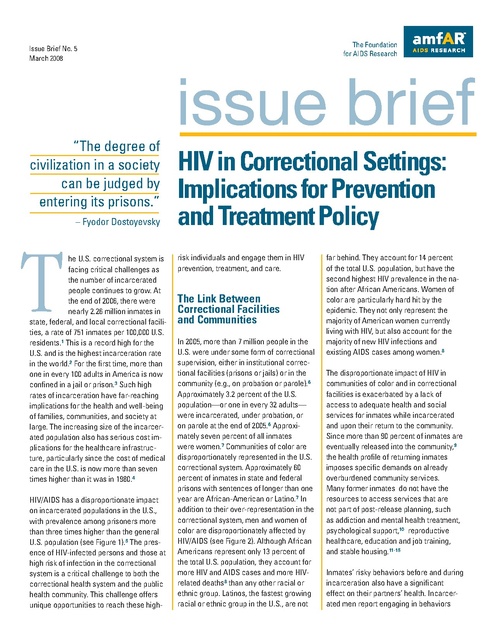
The Foundation for AIDS Research Issue Brief No. 5 March 2008 issue brief “The degree of civilization in a society can be judged by entering its prisons.” – Fyodor Dostoyevsky T he U.S. correctional system is facing critical challenges as the number of incarcerated people continues to grow. At the end of 2006, there were nearly 2.26 million inmates in state, federal, and local correctional facilities, a rate of 751 inmates per 100,000 U.S. residents.1 This is a record high for the U.S. and is the highest incarceration rate in the world.2 For the first time, more than one in every 100 adults in America is now confined in a jail or prison.3 Such high rates of incarceration have far-reaching implications for the health and well-being of families, communities, and society at large. The increasing size of the incarcerated population also has serious cost implications for the healthcare infrastructure, particularly since the cost of medical care in the U.S. is now more than seven times higher than it was in 1980.4 HIV/AIDS has a disproportionate impact on incarcerated populations in the U.S., with prevalence among prisoners more than three times higher than the general U.S. population (see Figure 1).5 The presence of HIV-infected persons and those at high risk of infection in the correctional system is a critical challenge to both the correctional health system and the public health community. This challenge offers unique opportunities to reach these high- HIV in Correctional Settings: Implications for Prevention and Treatment Policy risk individuals and engage them in HIV prevention, treatment, and care. The Link Between Correctional Facilities and Communities In 2005, more than 7 million people in the U.S. were under some form of correctional supervision, either in institutional correctional facilities (prisons or jails) or in the community (e.g., on probation or parole).6 Approximately 3.2 percent of the U.S. population—or one in every 32 adults— were incarcerated, under probation, or on parole at the end of 2005.6 Approximately seven percent of all inmates were women.7 Communities of color are disproportionately represented in the U.S. correctional system. Approximately 60 percent of inmates in state and federal prisons with sentences of longer than one year are African-American or Latino.7 In addition to their over-representation in the correctional system, men and women of color are disproportionately affected by HIV/AIDS (see Figure 2). Although African Americans represent only 13 percent of the total U.S. population, they account for more HIV and AIDS cases and more HIVrelated deaths8 than any other racial or ethnic group. Latinos, the fastest growing racial or ethnic group in the U.S., are not far behind. They account for 14 percent of the total U.S. population, but have the second highest HIV prevalence in the nation after African Americans. Women of color are particularly hard hit by the epidemic. They not only represent the majority of American women currently living with HIV, but also account for the majority of new HIV infections and existing AIDS cases among women.8 The disproportionate impact of HIV in communities of color and in correctional facilities is exacerbated by a lack of access to adequate health and social services for inmates while incarcerated and upon their return to the community. Since more than 90 percent of inmates are eventually released into the community,9 the health profile of returning inmates imposes specific demands on already overburdened community services. Many former inmates do not have the resources to access services that are not part of post-release planning, such as addiction and mental health treatment, psychological support,10 reproductive healthcare, education and job training, and stable housing.11-15 Inmates’ risky behaviors before and during incarceration also have a significant effect on their partners’ health. Incarcerated men report engaging in behaviors Figure 1 Prevalence of HIV/AIDS in State and Federal Prisons and in the U.S. Population in 2005 2.0% In correctional settings In U.S. population 1.7% 1.5% 1.0% 0.5% 0.4% 0.31% the primary partner is released. Similarly, individuals who are released from correctional facilities may want to maintain friendships that were made while incarcerated and, therefore, introduce new members into an existing social or sexual network. The presence of concurrent sexual networks has been found to contribute to elevated rates of HIV infection in communities already affected by high STI rates and other social and health issues.19 Alcohol and drugs are often a part of the context in which risky sexual practices occur and, in one study of men just released from prison, were associated with risky sexual behavior at one week and at six months after release.20 In addition to sharing drug injection paraphernalia, other risks include engaging in sexual acts to obtain drugs or providing a partner with drugs as a way to obtain sex. 0.15% HIV in Correctional Settings 0.0% % with HIV/AIDS % with Confirmed AIDS Sources: a) HIV/AIDS (State and Federal Prisons): Maruschak LM. HIV in Prisons, 2005. Department of Justice. Bureau of Justice Statistics, NCJ 218915. September 2007. Available at: http://www.ojp.usdoj.gov/bjs/pub/pdf/hivp05.pdf. b) HIV/AIDS (U.S. Population): CDC. HIV/AIDS Surveillence Report: Cases of HIV Infection and AIDS in the United States and Dependent Areas, 2005. Volume 17, Revised June 2007. Available at www.cdc.gov/hiv/topics/surveillance/resources/reports/2005report/pdf/ 2005SurveillanceReport.pdf. that elevate their risk for HIV and other sexually transmitted infections (STIs) both before incarceration and after release.16 These behaviors include injection drug use, needle sharing, and unprotected sex with multiple high-risk partners.17 Since approximately 50 percent of men who have been incarcerated or have passed through the correctional system consider themselves to be in committed heterosexual relationships and intend to return to their partners upon release from custody,16 as many as 6.5 million women each year will experience the risk of having a partner who has been incarcerated.16 Given the disproportionate number of low-income men of color in correctional settings, low-income African-American and Latina women are more likely to have intimate sexual or needle-sharing relationships with recently imprisoned 2 men.16 Sexual risk behavior is not limited to those who are HIV negative; one study found that men with HIV who were released from prison had unprotected sexual intercourse within an average of six days of their release, and 31 percent of these men believed it was likely they would infect their primary sexual partner.18 It should be noted that inmates are not the only ones who engage in risk behaviors. The destructive impact of incarceration on existing partnerships, families, and communities may also facilitate new and varied sexual and social connections that further increase risk of HIV transmission for inmates returning to their communities. For example, individuals whose primary partners are incarcerated for long periods of time may develop other sexual relationships, which may continue even after The first report of AIDS in correctional facilities was published in the early 1980s.21,22 Currently, all U.S. state correctional facilities have reported inmates with HIV infection, and it is estimated that up to one-fourth of the people living with HIV in the U.S. pass through a correctional facility each year.23 Although the number of known HIV-positive inmates has been steadily decreasing since 1999, the overall rate of confirmed AIDS cases among the prison population (0.4 percent) at the end of 2005 was close to three times the rate in the general U.S. population (0.15 percent).5 Data from federal prisons show that in 2004, HIV infection rates were highest among African-American female inmates (2.6 percent); in both federal and state prisons, females were more likely than males to be HIV positive, and African Americans and Latinos were more likely than whites to be HIV positive.24 State and federal corrections data from 2005 indicate that African-American inmates accounted for two-thirds of the AIDS-related deaths while in custody; moreover, they were nearly 2.5 times more likely than whites and almost five times more likely than Latinos to die from AIDS.5 In addition to higher rates of HIV infection and AIDS, correctional populations also have higher rates of co-morbid conditions that facilitate HIV transmission, such as STIs, substance use, mental health problems, and other infectious diseases such as tuberculosis and hepatitis. Drug-dependent inmates are also more likely than other inmates to report experiences of sexual abuse, housing instability, unemployment, parental substance use, and parental incarceration. One in seven drug-dependent inmates in state prisons reported being homeless in the year before incarceration, which contributes to a lack of access to healthcare.25 Sexual Behavior Many individuals are already infected with STIs and other diseases (e.g., hepatitis C) by the time they arrive at a correctional facility. Due in part to participation in sex work, women may be at greater risk of entering prison with STIs.26 Researchers also demonstrated that risky sexual behaviors associated with STI and HIV transmission can occur during incarceration27,28 via sexual relations (both consensual and coerced) among inmates as well as between inmates and prison officials (e.g., correctional officers).20 Condom availability is rare except in a few state prisons and county jails. However, even when condoms are available, they are rarely used during consensual sex. In one study, only 30 percent of prisoners reported using condoms or improvised barrier methods during consensual sex; no barrier methods were used during rape.29 Although some of the sexual activity occurring in prisons may be consensual, the very context of life in correctional facilities is such that true consent may be illusory. Sexual activity may occur as a means of survival (e.g., obtaining goods or protection) or as a result of coercion. It is estimated that 20 percent of male inmates and 25 percent of female inmates face sexual assaults behind bars.30,31 While any inmate can become a victim of sexual assault, certain inmates are particularly vulnerable. Nonviolent, first-time offenders are more likely to be victimized, as are gay and transgender detainees and youth held in adult facilities.32 Immigrants are also vulnerable to sexual assault in Figure 2 Disproportionate Impact of AIDS and Incarceration on Minorities, 2005 100% Proportion of total U.S. AIDS cases, 2005 Proportion of correctional facility population Proportion of total U.S. population 90% 80% 70% 68% 60% 50% 50% 39.5% 40% 34.6% 30% 30% 20.2% 20% 18% 14% 13% 10% 5.7% 5% 2% 0% % White, Non-Latino % Black, Non-Latino % Latino % Other Sources: a) Ethnicity in Corrections: Harrison PM, Beck AJ. Prisoners in 2005. Department of Justice, Bureau of Justice Statistics Bulletin, NCJ215092, November 2006, Revised January 2007. Available at: www.ojp.usdoj.gov/bjs/pub/pdf/p05.pdf. b) Ethnicity in AIDS Cases and U.S. Population: CDC HIV/AIDS Surveillance by Race/Ethnicity (through 2005), Powerpoint slides revised June 28 2007. Available at: www.cdc.gov/hiv/topics/surveillance/resources/slides/race–ethnicity/index.htm. 3 prisons, due in part to fear of deportation, and limited literacy and language skills.32 Such assaults on immigrant prisoners might be prevented by increased monitoring of U.S. Immigration and Customs Enforcement (ICE) detention centers by immigrant advocacy organizations. Sexual violence in prisons and jails is drastically underreported. While legal protections exist to protect inmates from guard brutality and violence inflicted by other prisoners, sexual violence in prisons and jails is drastically underreported due to the illicit nature of the activity and the stigma associated with rape and same-sex behavior.33 Inmates’ unwillingness to report their victimization contributes to the failure of prison authorities to react appropriately and to investigate complaints of sexual violence. This limits authorities’ ability to prosecute perpetrators or to provide victims with appropriate access to care, including HIV testing, counseling, and post-exposure prophylaxis.33 Unsterile Injection Equipment Tattooing is a common practice in correctional settings and is associated with group membership and desire for personal expression. The use of unsterile, makeshift tattooing equipment (including guitar strings, pins, needles, etc.) is a risk factor for transmission of HIV, hepatitis, and other parenterally transmissible infections.34 Not surprisingly, these makeshift instruments are difficult to sterilize reliably,35 thus facilitating the spread of blood-borne infections. Possession and use of illicit substances are forbidden in correctional facilities, but research has found that such substance use prohibitions may be circumvented through the cooperation of correctional personnel.20,36 Due to a lack of new and sterile injection equipment, a large proportion of incarcerated drug users 4 who are using injection drugs share needles or are unable to clean them adequately.37 Mental Health Issues Mental health issues also contribute to HIV risk behavior. Data from 2005 show that 56 percent of state prisoners, 45 percent of federal prisoners, and 64 percent of jail inmates had been clinically diagnosed with mental illness exclusive of substance use or dependence.38 Women were more likely than men to be diagnosed with mental health problems, as were white inmates and those 24 years of age or younger. Compared to other inmates, those with mental health needs were more likely to report having lived in foster homes or institutions while growing up, histories of physical or sexual abuse, family members with histories of substance use and incarceration, and low rates of employment.38 Approximately three-fourths of the state prisoners and jail inmates who had mental health diagnoses also met criteria for substance use or dependence, and more than a third of inmates with mental health diagnoses reported having used drugs at the time of their offense.38 Further, mentally ill inmates are much more likely to suffer physical abuse while incarcerated, earn disciplinary sanctions for breaking prison rules, and to accrue further criminal punishment that lasts throughout their incarceration.39 The use of isolation as a form of discipline can exacerbate mental illness and prompt acts of self-harm.40 Improving HIV Services for Incarcerated Populations The period of incarceration provides a unique window of opportunity to reach both uninfected and HIV-positive inmates with targeted education about and services for HIV prevention, treatment, and care. This position is supported by domestic41,42 as well as international43,44 authorities on HIV prevention. Prevention A fundamental starting point for HIV prevention in any setting is knowledge of one’s HIV status. The Centers for Disease Control and Prevention (CDC) has recommended that correctional institutions routinely offer HIV testing as a component of standard medical evaluation for inmates.41,45 While policies for HIV testing vary by jurisdiction and by type of correctional facility,46 fewer than half of the state prison systems and few jails routinely provide HIV testing on entry.46 For many inmates in correctional facilities that offer or mandate HIV testing, incarceration represents the first real contact with a healthcare system,47 and may be the first time they have been offered HIV testing.48,49 Of the institutions that do currently provide HIV testing to inmates, some take the “no news is good news” approach to diagnostic testing and, thus, do not inform or counsel individuals with negative HIV and STI test results.49,50 This lack of follow-up for uninfected persons represents an important missed opportunity for prevention counseling that has serious implications. Receiving negative test results can create a critical “teachable moment” for inmates to receive sexual and drug use-related risk reduction education, acquire accurate prevention and care information, and reinforce risk reduction practices. Furthermore, because some inmates who test negative for HIV may actually be in the early stages of infection (before HIV antibodies have developed), it is critical to provide education about the importance of repeat testing. A major problem with standard HIV testing is the waiting period of two weeks or longer for blood samples to be analyzed and the results returned to the inmate. This issue is particularly relevant for correctional facilities that house inmates for shorter periods of time (such as jails) or that function as transfer facilities for inmates being relocated. In such facilities, waiting two weeks for a test result translates into missed opportunities for inmates to learn their serostatus and receive appropriate counseling and referrals to care. Rapid testing assays that allow the immediate provision of results may be a more viable option in these types of settings.51,52 Aside from the logistical issues, it is important to note that inmates themselves may have valid concerns about getting an HIV test while incarcerated. In addition to the stigma associated with HIV/AIDS, inmates may also be concerned that medical confidentiality will not be maintained. Moreover, inmates may be concerned that testing positive will result in housing segregation, ostracism by or violence from other inmates, and decreased access to medical care and support services. Despite these issues, offering repeat voluntary counseling and testing within correctional settings can be an important entry point to HIV-related prevention and care services for at-risk and infected inmates.50 Because inmates may be psychologically impaired due to substance use or trauma, care must be taken to ensure that they are ready to receive HIV test results and counseling. To maximize the uptake of HIV testing, correctional facilities should keep inmates’ medical information strictly confidential. Recognizing the benefits of routine testing in correctional institutions, leading public health organizations such as the CDC41 and the National Commission on Correctional Health Care53 agree that all HIV tests must be conducted with the inmate’s consent and that inmates should have the right to opt out of testing. Unfortunately, this agreement is not present in all correctional institutions: in 2003, 19 state prisons and the Federal Bureau of Prisons had mandatory HIV screening policies for their incoming inmates.54 While many prisoners are intellectually capable of giving informed consent, the context of being incarcerated and the omnipresent potential for coercion in correctional settings call into question the degree to which inmates are truly able to give free and informed consent. Routine HIV testing procedures must be undertaken in a fashion that allows inmates to be told of and to exercise their right to refuse testing and other medical care. Extreme care must be taken to ensure that refusal of testing does not result in adverse consequences or punishment. For example, a study of a pilot program implementing routine HIV testing in District of Columbia jails obtained reports from inmates stating that those refusing HIV testing were placed on “medical hold,” that is, confined in a single cell until they complied.55 Fortunately, this practice was discontinued as a result of strong negative responses from the local community and the uncertain legal standing of this procedure. Nonetheless, reports such as these imply that routine or “automatic” testing is hardly voluntary given the consequences of refusal. To maximize the uptake of HIV testing, correctional facilities should keep inmates’ medical information strictly confidential, and provide linkages and access to specialty care and support services. Correctional care providers in Rhode Island have reported that ensuring these important components of care has resulted in the vast majority of inmates— both positive and negative—accepting HIV testing services.56 Peer Education and Other Prevention Services for Inmates Because incarcerated populations are ethnically, culturally, and educationally diverse, HIV prevention and other health education programs must be designed in a way that effectively reaches diverse populations and addresses special needs. While education about HIV/AIDS preven- tion and care can and should be delivered by correctional health staff or outside service contractors, research shows that prevention education programs delivered by peer educators are highly effective in establishing the trust and rapport that are needed to discuss sensitive topics related to sexual practices, substance use, and HIV/AIDS.57 Because peer educators are often inmates or former inmates, they are more attuned to the realities of life both in the correctional facility and post-release and, thus, may be more successful in providing support and teaching the skills necessary to address the complicated situations that put inmates at risk.58 Moreover, peer educators may be able to motivate inmates more effectively to access HIV-related services. For example, one study found that 44 percent of inmates requested HIV testing after participating in a peer-led program, despite the fact that HIV testing in that facility was not anonymous and individuals diagnosed with HIV or AIDS were housed separately.59 Harm Reduction and Risks Related to Sexual Behavior and Substance Use Although sexual and substance use behaviors are not permitted in incarcerated settings, the reality is that such behaviors do occur. Therefore, efforts to reduce the risk of infection from these behaviors would benefit both the incarcerated persons and the communities to which they return. Indeed, researchers and advocates have expressed the need for more harm reduction programs in prisons and jails.60 While the use of harm reduction strategies such as condoms and access to sterile injection equipment in correctional facilities is endorsed by the World Health Organization,61 the vast majority of U.S. prisons and jails specifically prohibit the distribution and possession of these items.50 Condoms are currently provided on a limited basis in only two state prison systems (Vermont and Mississippi) and five county jail systems (New York, Philadelphia, San Francisco, Los Angeles, and Washington, D.C.∗).24 Contrary to critics’ arguments, * In Washington, D.C., only the public jail has limited condom distribution. The privately run correctional treatment facility bans condoms. 5 few inmates have used condoms as weapons or to smuggle contraband into correctional facilities11,62 and there is no evidence that sexual activity within correctional facilities has increased as an outcome of condom distribution.62,63 In fact, in those correctional institutions (both in the U.S. and elsewhere) where a condom availability program exists, there have been no security or custody issues that resulted in the closure of the program.64 With regard to substance use, harm reduction measures are relatively new to correctional systems and are often perceived as a threat to their security regulations and traditional abstinence-oriented drug policy.65 Currently, no correctional facilities in the U.S. provide sterile injection equipment to inmates. However, harm reduction programs related to injection drug use have been established in more than 50 prisons in eight European countries. Evaluations of such programs in Switzerland, Spain, and Germany found no increase in drug use, dramatic decreases in needle sharing, no new cases of HIV infection or hepatitis, and no reported instances of needles being used as weapons.64,65 Addressing Addiction and Mental Health Issues Over the past several decades, the number of drug-involved offenders incarcerated in state and federal penitentiaries has increased substantially as a result of more stringent drug-related laws.65 These laws, coupled with the inadequate availability of community-based substance use programs, have exacerbated the negative impact of the nation’s drug problem on families and communities without addressing the medical and socioeconomic roots of addiction. Incarceration can provide a unique opportunity to treat inmates with addiction and mental health diagnoses. However, such programs are limited in correctional settings. Estimates from 2004 indicate that, although 53 percent of state and 45.5 percent of federal inmates met diagnostic criteria for drug dependence, only 14.8 percent of state and 17.4 percent of federal inmates received professional 6 addiction treatment.25 Although such treatment programs can be costly, research has shown that investing in addiction treatment for inmates is costeffective66,67 and can result in substantial reductions in post-release criminal activity, relapse, and recidivism.67,68 Addressing Stigma and Discrimination Stigmatization of HIV/AIDS remains prevalent in correctional institutions. Individuals who enter with or test positive for HIV may face discrimination and threats from correctional officers and other inmates and can be segregated or denied prison jobs, activities, and visiting privileges.55 Some correctional authorities may believe that HIV-positive prisoners need to be isolated for their own safety. Others argue that segregating inmates with HIV is undesirable because it labels them unnecessarily, makes them more vulnerable to assault and discrimination, and may result in disparate treatment and diminished access to services and desirable housing conditions. In some cases, HIV-negative inmates may pressure correctional authorities to house HIV-positive inmates separately. The resulting false sense of security may lead to an increase in high-risk behaviors among a population that incorrectly assumes itself free of HIV infection.16 As a step toward reinforcing HIV prevention education and minimizing misinformation and stigma, both inmates and correctional staff need comprehensive HIV/AIDS education, including information about the importance of repeat HIV testing for those practicing high-risk behaviors.69 Treatment and Care for HIV-Positive Inmates The implementation of routine testing policies in correctional facilities has important implications for the correctional system’s identification and case management of HIV-positive inmates.70 Privacy and confidentiality concerns are significant barriers to HIV testing and care-seeking in correctional settings. Given the unique living conditions (and, in many cases, overcrowding) in correctional facilities, maintaining confidentiality of personal and/or medical information can be extremely difficult. While confidentiality may be breached by other inmates, other breaches of confidentiality may be due to inappropriate behaviors by correctional staff or procedures associated with accessing prison healthcare,71 by attending pill call or standing in the medication dispensing line,56 or simply from having to fill out forms requesting medical attention and the reasons for needing to see a clinician.72 Effective HIV treatment in prisons has led to a 75 percent reduction in AIDSrelated mortality. All inmates in correctional systems have a constitutional right to medical care, including HIV care. Given that about 75 percent of HIV-positive inmates initiate treatment while incarcerated,73 the opportunities for successful viral suppression and overall management of HIV disease can be improved through increased adherence to a well-designed care system. Indeed, effective HIV treatment in prisons has led to a 75 percent reduction in AIDS-related mortality, a decline mirroring that of nonincarcerated populations.74,75 Some have alleged that HIV care and support in the correctional setting lags behind the standards in the community due to cost concerns, lack of adequately trained care providers, and stigmatization of HIV/AIDS.69 Privatization of correctional healthcare has imposed further constraints on HIV care delivery.76 The increased prevalence of HIV in correctional populations indicates the need for greater attention to HIV/AIDS prevention, case management and care in correctional facilities,77 as well as attention to treating the co-morbid conditions (e.g., hepatitis, TB, addiction) that could negatively affect therapeutic outcomes. One factor contributing to inadequate healthcare for inmates is the lack of coordination and programming within correctional institutions, and between correctional institutions and healthcare providers in the community. Correctional medical providers are not routinely given access to information about the HIV status of individuals under their care.50 Certain aspects of incarceration—such as “lock down” periods, punitive detentions, court appearances, and transfers between facilities—also undermine consistent dosing schedules essential to the longterm effectiveness of antiretroviral and other medications. Additionally, some state correctional facilities require inmates to provide “co-payments” for medical services;53,72 inmates who cannot pay may be reluctant to seek those services for fear of being rejected. Correctional administrators in the U.S. are increasingly concerned about the escalating costs of healthcare for “special needs” inmates, such as drug users and those with HIV.78 In some cases, correctional staff with no specialized training in HIV, drug or alcohol addiction, or mental illness are the ones obligated to provide care. For example, in 2000, two-thirds of all inmates receiving psychotherapy or medications were in facilities that did not specialize in providing mental health services.79 Medical providers have reported missed opportunities for linkages with the public health systems in the community after offenders are released.50 In some cases, the lack of coordination is due to confidentiality-related policies pertaining to the sharing of patient information across different agencies.12 In other cases, poor coordination is due to inadequate staffing levels and insufficient resources for discharge planning.12 Correctional health and public health authorities should work together to develop cost-effective mechanisms by which HIV-positive and other “special needs” inmates can receive appropriate and consistent treatment and care, both while they are incarcerated and upon release. Discharge Planning and Other Programs Following Release from Incarceration Each year, close to 700,000 prisoners are released from state and federal prisons.80 Post-release or discharge planning for this population is critical in ensuring continuity of HIV prevention, treatment, and care through linkages and access to necessary medical and psychosocial support services.12 Even in optimal cases, when inmates receive the care they need during their period of incarceration, the benefits achieved by this treatment are only sustainable if these same services are available and accessible to the inmates when they return to their communities.14 Discharge planning activities include providing inmates with information about outside resources, prescribing medications at release in sufficient quantity, scheduling and accompanying inmates to appointments with care providers, and assisting with applying for medical and financial assistance. Offenders with HIV/AIDS have admitted to seeking re-arrest to access medical services in prisons. Recent data pertaining to the health of exoffenders underscore the importance of appropriate post-release planning and linkages to care.81 A study of more than 30,000 newly released prison inmates found that, compared to the general population, former inmates’ risk of death was nearly 13 times higher during their first two weeks out of prison. Over the entire study period of 3.5 years, the adjusted death rate was 3.5 times higher than that of the general population, and the rates for every major cause of death (e.g., drug overdose, liver disease, suicide) were higher. To a large extent, death rates reflected the fact that the inmate population was poor and uneducated, and over 70 percent of the sample had been diagnosed with drug or alcohol dependence. Without appropriate pre-release planning or other similar support, newly released inmates may not be able to access lifesaving services such as addiction treatment, medical care, and transitional housing.81 For HIV-positive inmates, one of the greatest impediments to continuity of care is being released from a correctional facility without knowing their HIV status or what their treatment options are.70 A study examining the response to antiretroviral treatment in the correctional setting indicated that, when provided with adequate clinical care, inmates have clinical improvements that are comparable to those found in the community.82 Without appropriate discharge planning, the benefits of antiretroviral treatment that may have been achieved during incarceration may be lost after returning to the community.82 Moreover, applying for federal and state medical assistance can take several months, leaving qualified ex-offenders without access to necessary healthcare and financial support in the critical period after release.13 Offenders with HIV/AIDS have admitted to seeking re-arrest to access medical services in prisons, which highlights the crucial need for such services for released offenders.14 Continuity in HIV treatment and care for ex-inmates is also hampered by lack of access to health insurance. Many exoffenders do not have private sources of healthcare coverage and must rely on public programs, free clinics, and emergency rooms to receive medical attention.83 Moreover, gaining access to public health insurance can be equally difficult. Although federal regulations do not require termination of inmates’ Medicaid eligibility upon incarceration, a 1999 survey found that all 50 states had policies terminating inmates’ Medicaid coverage upon incarceration.84 For those with terminated Medicaid benefits, the process of re-establishing eligibility can take anywhere from 14 to 45 days (and sometimes longer), depending on the state.85 7 The Center for Medicaid and State Operations has encouraged states to suspend rather than terminate inmates’ Medicaid benefits during the period of incarceration to ensure that benefits are restored to eligible individuals immediately upon release.86 Making reinstatement to Medicaid eligibility a fundamental component of discharge planning would contribute to successful re-entry85 and would ensure that ex-offenders have access to essential healthcare services.83 Discharge planning programs focusing on HIV prevention have been found to have significant, positive effects on sexual risk behavior. Despite these barriers, some correctional systems have tried to reduce the likelihood of ex-offenders falling through the cracks when trying to access care by establishing partnerships with community health providers. These independent efforts enable correctional health facilities to have medical staff who also work in the community, common medical records systems, and well-developed referral and outreach protocols.87 Federal funds received under the Ryan White CARE Act (RWCA), as established in Title XXVI of the Public Health Service Act, allow community-based organizations to provide short-term traditional support services, such as linkages to primary care, to HIV-positive inmates prior to release and as part of effective discharge planning.88 It is important to note that RWCA funds can be used only where no other services exist, or where these services are not the responsibility of the correctional system.88 Some correctional facilities have also tried to address the limitations of the 8 current system by establishing enhanced discharge planning for inmates. Compared to standard processes, enhanced discharge planning incorporates planning for a variety of inmates’ needs, such as healthcare, mental health treatment, treatment of addiction, housing, and employment. Existing discharge planning programs focusing on HIV prevention have been found to have significant, positive effects on sexual risk behavior,89,90 while programs focusing on the needs of HIVpositive inmates have been successful in retaining a very challenging population in care and addressing their needs for both HIV medical care and addiction treatment without providing any of these services directly.91 Addressing these important prevention and healthcare needs in advance of release from incarceration could greatly enhance successful transition to the community. Removing Social Policy Barriers to Successful Re-Entry Providing access to adequate health and social services to ex-offenders upon release would address the current gaps in continuity of care for those in need of HIV services. However, the provision of healthcare alone is insufficient to address the complex social and economic issues that contribute to the high prevalence of HIV among corrections populations and minorities. Current policies that make it difficult for ex-offenders to find adequate housing and employment, and to gain access to public assistance, only serve to exacerbate the impact of HIV in these populations, particularly low-income communities of color. For example, in most states, individuals are released from correctional facilities without the documentation necessary to obtain a state-issued identification card, and many states do not accept prison documentation as valid proof of identity.92 Without some sort of government identification, ex-inmates are unable to complete the application processes for a variety of essential medical and health services, such as obtaining Social Security benefits, public or private healthcare coverage, and other public assistance. In addition, proof of identity is often a necessary requirement for completing job applications, and is absolutely required to cash paychecks or open bank accounts. The simple act of ensuring that all inmates have the appropriate identification documentation upon release may greatly enhance their ability to make a successful transition back to the community. Lack of identification is not the only barrier to getting a job for former inmates. In fact, very few ex-offenders have jobs waiting for them when they return to their communities and the majority of others face significant barriers to getting employment due to lack of job skills, lack of education, and employers’ unwillingness to hire individuals with criminal records.93 Although most corrections facilities offer some type of educational program or vocational training for inmates, there are only a limited number of program slots.94,95 This lack of slots is unfortunate given that the existing data indicate that such programs are associated with improved outcomes, including reduced criminal recidivism.96,97 Even when such programs are available, however, HIV-positive inmates may not be granted access to them. The Alabama Department of Corrections, for instance, bars HIVpositive state prisoners from participating in community-based programs such as work release.98 However, a recent change in the Department of Corrections’ policies now allows HIV-positive prisoners to participate in transitional programs involving education and vocational training.99 Ensuring that ex-offenders and their families have sufficient social and economic support may help prevent them from participating in illegal activities as a means of support, or engaging in behaviors such as drug use that increase their risk for HIV. In order to support themselves and their families, many ex-offenders turn to public assistance. However, obtaining such support can be problematic. The Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (which instituted the Temporary Assistance for Needy Families [TANF] Act; P.L. 104-193) stipulates that persons convicted of a state or federal felony drug conviction are subject to a lifetime ban on eligibility for food stamps and other benefits. While this policy has a direct effect on individual inmates’ ability to rebuild their own lives, it also has a substantial impact on inmates’ ability to support their children and families. Because formerly incarcerated men have diminished earning capacity (as much as 40 percent less) over the course of their lifetimes, they are unable to provide as much support to the families with whom they live.100 Hence, a vicious cycle is perpetuated: the communities from which inmates come are places with very few economic resources, and inmates returning to these communities are unable to contribute to the economic stability of the community due to diminished earning potential. The result is diminished family health and well-being, as well as weakened family stability.101 Furthermore, because of the demographic profile of incarcerated persons with felony drug convictions, this policy has a disproportionate impact on African-American and Latina women, as well as AfricanAmerican men—populations already experiencing significant social and health disparities, including greater risk of HIV infection.93 Revising this policy to reinstate eligibility for benefits to those with felony drug convictions—for example, after some prescribed period of time and after proof of rehabilitation—could have a positive impact on ex-offenders and their families, who are trying to re-establish stable lives in their communities. Lack of employment, income, and access to public assistance all contribute to housing instability for ex-offenders and their families. Given the links between housing instability and health outcomes (such as HIV risk, mental illness, and addiction), ensuring resources for and linkages to stable housing for newly released individuals is another critical step to successful re-entry. Research has shown that inability to secure stable housing and employment after release from prison may lead drug-involved ex-offenders back to drug dealing and to risks associated with this lifestyle, including risky sexual behaviors.60,102,103 Federal legislation (such as the Department of Housing and Urban Development’s Housing Opportunity Program Extension Act of 1996) restricts or, in some cases, denies access to public housing for many exoffenders, particularly those convicted of drug-related offenses.93,95 While some exoffenders may try to find housing with family members or friends, such efforts may not always be successful. If family members or friends reside in public housing, accepting an ex-offender into their home may jeopardize their own residential stability due to the exclusion policies applicable to federally subsidized housing. For inmates with HIV, access to stable housing can be the critical factor in maintaining HIV treatment adherence. While the lack of affordable housing is a problem for the general population, making efforts to link newly released inmates with affordable, stable housing has been shown to reduce rates of recidivism.104,105 For those inmates with HIV or at risk of infection, access to stable housing can be the critical factor in maintaining HIV treatment adherence and risk reduction behaviors, increasing access to medical services, and improving health outcomes.106-108 Incorporating efforts to secure stable housing as a part of effective discharge planning for soon-to-be-released inmates could help to reduce recidivism and ensure that any health-related gains achieved during incarceration are not reversed once individuals are back in their communities. Conclusion As a result of poverty, addiction, and other forms of health and social disenfranchisement in their home communities, inmates in correctional facilities have a uniquely high prevalence of communicable disease, including HIV/AIDS.109 In some ways, this is not surprising given that, in almost every corner of the world, HIV strikes the communities that are the least economically and politically empowered.110 The disparities observed in America’s correctional system reflect some of the problems seen in its healthcare system. A strong commitment from all sectors of society is needed to reduce social and economic disparities in both systems in order to enhance the health and well-being of all Americans, regardless of race or ethnicity. While it may seem that the goals of the public health and corrections communities are worlds apart, the reality is that both strive to improve the conditions in society that enhance public safety and contribute to overall quality of life. Given the multidimensional impact of HIV/AIDS on individuals and families, the public health and corrections/criminal justice communities should work more collaboratively to address the socioeconomic disparities and environmental factors that put individuals at risk for both HIV infection and incarceration. Prison health is public health.111 In order to alleviate the devastating impact of HIV/AIDS on communities that are already disproportionately affected by the epidemic, it is imperative to address the individual, social, and environmental factors that predispose members of these communities to both HIV risk and risk of incarceration. It is equally imperative that we take full advantage of the window of opportunity provided by incarceration to give inmates access to the healthcare and social services that could facilitate reductions in morbidity and mortality, successful reentry, and decreased recidivism. Doing so would not only benefit the health of incarcerated persons, but also their families and communities. 9 References 1. Sabol JS, Couture H, Harrison PM. Prisoners in 2006. Bureau of Justice Statistics. December 2007 (NCJ 219416). Available at: http://www.ojp.usdoj.gov/bjs/pub/pdf/p06.pdf. 2. Ringer R. U.S. Incarcerates More People Than Any Other Country. Human Rights Watch News and Releases, December 6, 2007. Available at: http://bbsnews.net/article.php/20071206234320922. 3. Pew Center on the States. One in 100: Behind Bars in America 2008. February 2008. Available at: http://www.pewcenteronthestates.org/uploadedFiles/One%20in%20100.pdf. 4. Kaiser Family Foundation. Trends and Indicators in the Changing Health Care Marketplace. 2006. Available at: http://www.kff.org/insurance/7031/print-sec5.cfm. 5. Maruschak LM. HIV in Prisons, 2005. Washington, D.C.: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics Bulletin. September 2007. NCJ 218915. Available at: http://www.ojp.usdoj.gov/ bjs/pub/pdf/hivp05.pdf. 6. Glaze LE, Bonczar, TP. Probation and Parole in the United States, 2005. Washington, D.C.: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics Bulletin. NCJ 215091 2006. Available at: http://www.ojp.usdoj.gov/bjs/pub/ pdf/ppus05.pdf. 7. Harrison PM, Beck AJ. Prisoners in 2005. Washington, D.C.: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics Bulletin. November 2006. NCJ 215092. Available at: http://www.ojp.usdoj.gov/bjs/pub/pdf/p05.pdf. 8. Centers for Disease Control and Prevention (CDC). HIV/AIDS Surveillance Report 2005. Volume 17. Rev ed. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. June 2007. Available at: http://0-www.cdc.gov.mill1.sjlibrary.org/hiv/topics/surveillance/resources/reports/2005report/pdf/2005SurveillanceReport.pdf. 9. MacGowan RJ, Margolis A, Gaiter J, Morrow K, Zack B, Askew J, McAuliffe T, Sosman JM, Eldridge GD. Predictors of Risky Sex of Young Men after Release from Prison. International Journal of STD & AIDS. 2003;14(8):519–523. 10. American College of Physicians, National Commission on Correctional Health Care, American Correctional Health Care, American Correctional Health Service Association. The Crisis in Correctional Health Care: The Impact of the National Drug Control Strategy on Correctional Health Services. Annals of Internal Medicine. 1992;117:71–81. 11. Leh SK. HIV Infection in U.S. Correctional Systems: Its Effect on the Community. J Community Health Nurs. 1999;16(1):53–63. 12. Hammett TM, Roberts C, Kennedy S. Health-Related Issues in Prisoner Reentry. Crime & Delinquency. 2001;47(3):390–409. 13. Roberts C, Kennedy S, Hammett TM. Linkages Between In-Prison and Community-Based Health Services. Journal of Correctional Health Care. 2004;10(3):333–368. 14. De Devereux PG, Whitley R, Ragavan A. Discharge Planning for Inmates with HIV/AIDS: Can It Help Increase Adherence to Medical Treatment and Lower Recidivism? Corrections Today. 2002:127–29. 15. Grinstead O, Zack B, Faigeles B. Reducing Postrelease Risk Behavior among HIV Seropositive Prison Inmates: The Health Promotion Program. AIDS Education and Prevention. 2001;13(2):109–119. 16. Grinstead OA, Faigeles B, Comfort M, Seal D, Nealey-Moore J, Belcher L, Morrow K. HIV, STD, and Hepatitis Risk to Primary Female Partners of Men Being Released from Prison. Women & Health. 2005;41(2):63– 80. 17. Morrow KM, Eldridge G, Nealey-Moore J. Grinstead O. HIV, STD and Hepatitis Risk of the Week Following Release from Prison: An Event Level Analysis. Journal of Correctional Health Care. 2007;13(1):27–38. 18. Thomas JC, Torrone E. Incarceration as Forced Migration: Effects on Selected Community Health Outcomes. American Journal of Public Health. 2005;96(10):1762– 1765. 19. Adimora AA, Schoenbach VJ. Social Context, Sexual Networks, and Racial Disparities in Rates of Sexually Transmitted Infections. Journal of Infectious Diseases. 2005;191 (Suppl 1):S115–S122. 20. Seal DW, Belcher L, Morrow K, Eldridge G, Binson D, Kacanek D, Margolis AD, McAuliffe T, Simms R. A Qualitative Study of Substance Use and Sexual Behavior Among 18to 29-Year-Old Men While Incarcerated in the United States. Health Education & Behavior. 2004;31(6):775–89. 21. Hanrahan JP, Wormser GP, Maguire GP, Delorenzo LJ, Gavis G. Opportunistic Infections in Prisoners. New England Journal of Medicine. 1982;307(8):498. 22. Wormser GP, Krupp LB, Hanrahan JP, Gavis G, Spira TJ, Cunningham-Rundles S. Acquired Immunodeficiency Syndrome in Male Prisoners. New Insights into an Emerging Syndrome. Annals of Internal Medicine. 1983;98(3):297–303. 23. Spaulding AC, Stephenson B, Macalino G, Ruby W, Clarke JG, Flanigan TP. Human Immunodeficiency Virus in Correctional Facilities: A Review. Clinical Infectious Diseases. 2002;35(3):305–312. 24. Maruchak LA. HIV in Prisons, 2004. Washington, D.C.: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics Bulletin. November 2006. Available at: http://www.ojp.usdoj.gov/bjs/pub/pdf/hivp04.pdf. 25. Mumola CJ, Karberg JC. Drug Use and Drug Dependence, State and Federal Prisoners, 2004. Bureau of Justice Statistics Bulletin. U.S. Department of Justice, Office of Justice Programs. October 2006. NCJ 213530 2006. Available at: http://www.ojp.usdoj.gov/bjs/pub/pdf/dudsfp04.pdf. 26. Messina N, Grella C. Childhood Trauma and Women's Health Outcomes in a California Prison Population. American Journal of Public Health. 2006;96(10):1842–1848. 27. Wolfe MI, Xu F, Patel P, O'Cain M, Schillinger JA, St Louis ME, Finelli L. An Outbreak of Syphilis in Alabama Prisons: Correctional Health Policy and Communicable Disease Control. American Journal of Public Health. 2001;91(8):1220–1225. 28. Wohl AR, Johnson DF, Lu S, Jordan W, Beall G, Currier J, Simon PA. HIV Risk Behaviors among African American Men in Los Angeles County Who SelfIdentify as Heterosexual. Journal of Acquired Immune Deficiency Syndrome. 2002;31(3):354– 360. 29. Centers for Disease Control and Prevention (CDC). HIV Transmission Among Male Inmates in a State Prison System—Georgia, 1992–2005. Morbidity and Mortality Weekly Report. 2006;55(15):421–426. 30. Struckman-Johnson C, Struckman-Johnson D. Sexual Coercion Reported by Women in Three Midwestern Prisons. Journal of Sex Research. 2002;39(3):217–227. 10 31. Struckman-Johnson C, Struckman-Johnson D. Sexual Coercion Rates in Seven Midwestern Prison Facilities for Men. The Prison Journal. 2000:379–390. 32. Stop Prisoner Rape. In the Shadows: Sexual Violence in U.S. Detention Facilities. Report Prepared for the 36th Session on the U.N. Committee Against Torture. 2006. Available at: http://www.spr.org/pdf/in_the_shadows.pdf. 33. Human Rights Watch. No Escape: Male Rape in U.S. Prisons. April 2001. Available at: http://www.hrw.org/reports/2001/prison/report.html. 34. Centers for Disease Control and Prevention. Hepatitis B Outbreak in a State Correctional Facility. Morbidity and Mortality Weekly Report. 2001;50(MM25):529. 35. Day RF. Tatooing in Prison: An Innocuous Practice or a Conduit for Hepatitis C? The Body. June 2005. Available at: http://www.thebody.com/content/ art30800.html. 36. Talvi SJA. Women Behind Bars: The Crisis of Women in the U.S. Prison System. Emeryville, CA: Seal Press, 2007. 37. Gaughwin M, Douglas RM, Wodak AD. Behind Bars— Risk Behaviors for HIV Transmission in Prison, A Review. In HIV/AIDS and Prisons. AIC Conference Proceedings. 89–107. Available at: http://www.aic.gov.au/publications/proceedings/04/gaughwin.pdf. 38. James DJ, Glaze LE. Mental Health Problems of Prison and Jail Inmates. Bureau of Justice Statistics Bulletin. U.S. Department of Justice, Office of Justice Programs. September 2006. Available at: http://www.ojp.usdoj.gov/bjs/pub/pdf/mhppji.pdf. 39. U.S. Department of Justice, Civil Rights Division, 1997 CRIPA investigation into the conditions at Los Angeles County jail established that mental health care at the jail violated the inmate's constitutional rights. It found "unconstitutional conditions exist at the Los Angeles County Jail, including deliberate indifference to inmates' serious mental health needs." They found "abuse of mentally ill inmates by sheriff's deputies working in the jail: some have their illnesses misdiagnosed and their medications improperly administered. ... they have been abused by correctional staff; the jail does not adequately prevent abuse of mentally ill inmates and does not adequately investigate allegations of such abuse when it occurs." Paz RS. Accommodating Disabilities in Jails and Prisons. In: Greiginfer R, ed. Public Health Behind Bars: From Prisons to Communities. New York: Springer; 2007: 42–55. 40. Madrid vs. Gomez, 190 F.3d 990 (9th Cir. 1999). Paz RS. Accommodating Disabilities in Jails and Prisons. In: Greiginfer R, ed. Public Health Behind Bars: From Prisons to Communities. New York: Springer; 2007: 42–55. 41. Centers for Disease Control and Prevention (CDC). Advancing HIV Prevention: Interim Technical Guidance for Selected Interventions. April 2003. Available at: http://www.cdc.gov/hiv/topics/prev_prog/ AHP/resources/guidelines/pdf/ AHP IntGuidfinal.pdf. 42. Institute of Medicine. No Time to Lose: Getting More from HIV Prevention. Washington, D.C.: National Academies Press; 2001. 43. UNAIDS. International Guidelines on HIV/AIDS and Human Rights. Article 21(e). 2006. Available at: http://data.unaids.org/Publications/IRC-pub07/jc1252-internguidelines_en.pdf. 44. United Nations Office on Drugs and Crime. HIV/AIDS Prevention, Care, Treatment and Support in Prison Settings: A Framework for an Effective National Response. 2006. Available at: http://www.unodc.org/pdf/HIVAIDS_prisons_July06.pdf. 45. Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, Clark JE. Revised Recommendations for HIV Testing of Adults, Adolescents, and Pregnant Women in Health-Care Settings. Morbidity and Mortality Weekly Report. 2006;55(RR-14):1–17. 46. Hammett TM, Harmon P, Maruchak LM. 1996-1997 Update: HIV/AIDS, STDs and TB in Correctional Facilities. Washington, D.C.: U.S. Department of Justice, National Institute of Justice. July 1999. 47. Boutwell A, Rich JD. HIV Infection Behind Bars. Clinical Infectious Diseases. 2004;38(12):1761–1763. 48. Dixon PS, Flanigan TP, DeBuono BA, Laurie JJ, De Ciantis ML, Hoy J, Stein M, Scott HD, Carpenter CC. Infection with the Human Immunodeficiency Virus in Prisoners: Meeting the Health Care Challenge. The American Journal of Medicine. 1993;95(6):629–635. 49. Kacanek D, Eldridge GD, Nealey-Moore J, MacGowan RJ, Binson D, Flanigan TP, Fitzgerald CC, Sosman JM. Young Incarcerated Men's Perceptions of and Experiences with HIV Testing. American Journal of Public Health. 2007;97(7):1209–1215. 50. Grinstead OA, Seal DW, Wolitski R, Flanigan T, Fitzgerald C, Nealey-Moore J, Askew J. HIV and STD Testing in Prisons: Perspectives of In-Prison Service Providers. AIDS Education & Prevention. 2003;15(6):547–560. 51. Tinsley M, Kennedy S, Hammett T, Norton G, Spaulding A, Arriola KRJ. Key Issues in HIV Testing in Jails: Rapid Testing and Linkage to Care and Evaluation. Powerpoint presentation presented at the Academic and Health Policy Conference on Correctional Health Care. 2007. 52. Parece MS, Herrera GA, Voigt RF, Middlekauff SL, Irwin KL. STD Testing Policies and Practices in U.S. City and County Jails. Sexually Transmitted Diseases. 1999;26(8):431–437. 53. National Commission on Correctional Health Care (NCCHC). Position Statement: Administrative Management of HIV in Correctional Institutions. Adopted by the NCCHC Board of Directors on November 8, 1987, Revised October 9, 2005. Available at: http://www.ncchc.org/resources/statements/admin_hiv2005.html. 54. Kantor E. HIV Transmission and Prevention in Prisons. April 2006. Available at: http://hivinsite.ucsf.edu/ InSite?page=kb-07-04-13. 55. DC Appleseed Center for Law and Justice. Briefing Paper on HIV Testing in Jails. July 2006. Available at: http://www.dcappleseed.org/projects/publications/ HIVTestingJails.pdf. 56. Personal communication with Josiah Rich, Brown University, October 26, 2007. 57. Robillard AG, Garner JE, Laufer FN, Ramadan A, Barman TA, Devore BS, Myers JJ, Porterfield J, Wood PH. Centers for Disease Control and Prevention/Health Resources and Services Administration. HIV/AIDS Intervention, Prevention and Continuity of Care Demonstration Project for Incarcerated Individuals Within Correctional Settings and Community: Part I, A Description of Corrections Demonstration Project Activities. Journal of Correctional Health Care. 2003;9(4):453–486. 58. Grinstead OA, Faigeles B, Zack B. The Effectiveness of Peer HIV Educa- tion for Male Prisoners Entering State Prison. Journal of Health Education. 1997;28:S31–S37. 59. Grinstead OA, Zack B, Faigeles B. Collaborative Research to Prevent HIV among Male Prison Inmates and their Female Partners. Health Education & Behavior. 1999;26(2):225–238. 60. Seal DW, Margolis AD, Sosman J, Kacanek D, Binson D. HIV and STD Risk Behavior Among 18- to 25-Year-Old Men Released from U.S. Prisons: Provider Perspectives. AIDS Behavior. 2003;7(2):131–141. 61. World Health Organization. Policy Brief: Reduction of HIV Transmission in Prisons, 2004. May 2004. Available at: http://www.emro.who.int/aiecf/web34.pdf. 62. Center for Health Justice. In Custody Programming. Treatment and Prevention Education, Prisoner Hotline, Condom Distribution. Not Dated. Available at: http://healthjustice.net/incustody_programming.html. 63. Human Rights Watch. Ensure Access to Condoms in U.S. Prisons and Jails. March 2007. Available at: http://hrw.org/backgrounder/hivaids/condoms0307/. 64. Dolan K, Rutter S, Wodak AD. Prison-Based Syringe Exchange Programmes: A Review of International Research and Development. Addiction. 2003;98:153–158. 65. Okie S. Sex, Drugs, Prisons, and HIV. New England Journal of Medicine. 2007;356(2):105–108. 66. Daley M, Love CT, Shepard DS, Petersen CB, White KL, Hall FB. Cost-Effectiveness of Connecticut's In-Prison Substance Abuse Treatment. Journal of Offender Rehabilitation. 2004;39(3):69–92. 67. Belenko S. Behind Bars: Substance Abuse and America's Prison Population. New York: National Center on Addiction and Substance Abuse at Columbia University. 1998. Available at: http://www.casacolumbia.org/pdsopprov/ files/5745.pdf. 68. Spaulding AC, Weinbaum CM, Lau DT, Sterling R, Seeff LB, Margolis HS, Hoofnagle JH. A Framework for Management of Hepatitis C in Prisons. Annals of Internal Medicine. 2006;144(10):762–769. 69. DeGroot AS. Shedding Light on Correctional HIV Care. AIDS Reader. 2000;10(5):285–286. 70. Arriola JRJ, Braithwaite RL, Kennedy S, Hammett TM, Tinsley M, Wood P, Adcoleda C. A Collaborative Effort to Enhance HIV/STI Screening in Five County Jails. Public Health Reports. Washington, D.C.: U.S. Department of Health and Human Services 2001;116:520. 71. Personal communication, The D.C. Prisoners’ Project of the Washington Lawyers' Committee for Civil Rights and Urban Affairs. John Doe v. District of Columbia, et al: In partnership with the former D.C. Prisoners' Legal Services Project (now the D.C. Prisoners' Project of the Committee), the law firm of Patton Boggs litigated an important case in which the client was an HIV-positive man held in the privately-run Corrections Corporation of America Correctional Treatment Facility (CCA/CTF) in the District of Columbia. The client's privacy claims survived motions to dismiss in the Federal courts and a motion for summary judgment in the D.C. Superior Court. The case was scheduled for trial when it settled in 2006. Diligent discovery and investigation revealed questionable practices at the jail facility that arguably failed to safeguard prisoners' medical privacy. The litigation also unearthed evidence that a corrections officer may have posted the client's personal medical information on a bulletin board in the jail. As a result, the client endured a steady stream of violent threats and harassment and had his bed burned by other inmates. The case has increased in significance since it was filed in 2001, highlighting the critical importance of confidentiality protections as the District instituted a policy of routine HIV testing for all jail inmates in 2006. 72. Restum ZG. Public Health Implications of Substandard Correctional Health Care. American Journal of Public Health. 2005;95(10):1689–1691. 73. Altice FL, Mostashari F, Friedland GH. Trust and the Acceptance of and Adherence to Antiretroviral Therapy. Journal of Acquired Immune Deficiency Syndrome. 2001;28(1):47–58. 74. Baham J, Bick J, Giannoni D, et al. Trends in an HIV-Infected Incarcerated Population: An Autopsy Review. 2004. 40th Annual Meeting of the Infectious Diseases Society of America. 75. Bick J, Dewsnup D. Successful Primary Prophylaxis of Tuberculosis (TB) in HIV-Infected Persons with CD4<100 in a Correctional Setting. 1997. 35th Annual Meeting of the Infectious Disease Society of America. 76. DeGroot AS, Hammett TM, Scheib R. Barriers to Care of HIV-Infected Inmates: A Public Health Concern. AIDS Reader. 1996;6(3):78–87. 77. Chen JL, Callahan DB, Kerndt PR. Syphilis Control Among Incarcerated Men Who Have Sex With Men: Public Health Response to an Outbreak. American Journal of Public Health. 2002;92(9):1473– 1474. 78. Webster JM, Leukefeld CG, Tindall MS, Hiller ML, Garrity TF, Narevic E. Lifetime Health Services Use by Male Drug-Abusing Offenders. The Prison Journal. 2005;85:50–64. 79. Beck AJ, Maruchak LM. Mental Health Treatment in State Prisons, 2000. Washington, D.C.: U.S. Department of Justice, Bureau of Justice Statistics. July 2001. Available at: http://www.ojp.usdoj.gov/ bjs/abstract/mhtsp00.htm. 80. Sabol WJ, Harrison PM. Prison and Jail Inmates at Midyear 2006. Washington, D.C.: U.S. Department of Justice, Bureau of Justice Statistics. June 2007. Available at: http://www.ojp.usdoj.gov/bjs/pub/pdf/pjim05.pdf. 81. Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, Koepsell TD. Release from Prison — A High Risk of Death for Former Inmates. New England Journal of Medicine. 2007;356(2):157–165. 82. Springer SA, Pesanti E, Hodges J, Macura T, Doros G, Altice FL. Effectiveness of Antiretroviral Therapy among HIV-Infected Prisoners: Reincarceration and the Lack of Sustained Benefit after Release to the Community. Clinical Infectious Diseases. 2004;38(12):1754–1760. 83. McCorkel JA, Butzin CA, Martin SS, Inciardi JA. Use of Health Care Services in a Sample of Drug-Involved Offenders: A Comparison with National Norms. American Behavioral Scientist. 1998;41(8):1079–1090. 84. Lackey C. Council of State Governments. Final Results of State Medicaid Agencies Survey in Memorandum to Fred Osher, Director of Center for Behavioral Health, Justice and Public Safety. (October 16, 2000). New York, NY: Council of Statement Governments. 85. Bazelon Center for Mental Health Law. Finding the Key to Successful Transition from Jail to the Community: An Explanation of Federal Medicaid and Disability Program Rules (Washington, D.C.; Bazelon Center: 2001). 86. Letter from Glenn Stanton, Acting Director, Center for Medicaid and State Operations, to State Medicaid Directors and CMS Associate Regional Administrators for Medicaid. May 2004. 87. Freudenberg N. Community Health Services for Returning Jail and Prison Inmates. Journal of Correctional Health Care. 2004;10(3):369–397. 88. Health Resources and Services Administration. HIV/AIDS Bureau. Policy Notice—0101, The Use of Ryan White CARE Act Funds for Transitional Social Support and Primary Care Services for Incarcerated Persons. July 23, 2001. Available at: http://hab.hrsa.gov/ law/0101.htm. 89. Wolitski RJ. Relative Efficacy of a Multisession Sexual Risk-Reduction Intervention for Young Men Released from Prisons in Four States. American Journal of Public Health. 2006;96(10):1854–1861. 90. Myers J, Zack B, Kramer K, Gardner M, Rucobo G, Costa-Taylor S. Get Connected: An HIV Prevention Case Management Program for Men and Women Leaving California Prisons. American Journal of Public Health. 2005;95(10):1682–1684. 91. Health and Disability Working Group. Case Study: Project BRIDGE, Providence, Rhode Island. Boston University School of Public Health. 2003. Available at: http://www.bu.edu/hdwg/pdf/projects /trainingfiles/ProjectBridge.pdf. 92. National H.I.R.E. Network. Nationwide Survey of Identification Requirements for Newly Released Prisoners. September 2003. Available at: http://www.hirenetwork.org/ID_Survey_Summary.htm. 93. Williams NH. The Impact of Medicaid and Other Social Public Policy on African-American Men, Their Children and Families, Report dated July 2006 for Community Voices, National Center for Primary Care, Morehouse School of Medicine. Available at: http://aspe.os.dhhs.gov/medicaid/ july06/RoxanneLeopperAttachment1.pdf. 94. La Vigne NG et al. A Portrait of Prisoner Reentry in Maryland. Washington, D.C.: The Urban Institute Press; 2003. 95. Travis J. But They All Come Back: Facing the Challenges of Prisoner Re-Entry. Washington, D.C.: The Urban Institute Press; 2005. 96. Gaes GG et al. Adult Correctional Treatment. In: M. Tonry and J. Petersilia, eds. Prisons. Chicago, IL: University of Chicago Press; 1999. 97. Adams K et al. A Large-Scale Multidimensional Test of the Effect of Prison Education on Prisoners' Behavior. The Prison Journal. 2001;74(4):433–449. 98. Maddow R. Cost of Excluding Alabama State Prisoners with HIV/AIDS from Community-Based Programs. National Prison Project at ACLU Foundation, Inc., and Alabama Prison Project. April 2003. 99. Personal communication with Brian Corbett, Alabama Department of Corrections Public Information Manager, October 3, 2007. 100. Western B. Punishment and Inequality. New York: Russell-Sage; 2006. 101. Clear TR. Community Public Safety and Public Health. In: Greifinger R, ed. Public Health Behind Bars: From Prisons to Communities. New York: Springer; 2007: 13–24. 102. Kushel MB, Hahn JA, Evans JL, Bangsberg DR, Moss AR. Revolving Doors: Imprisonment Among the Homeless and Marginally Housed Population. American Journal of Public Health. 2005;95(10):1747–1752. 103. Freudenberg N, Daniels J, Crum M, Perkins T, Richie BE. Coming Home from Jail: The Social and Health Consequences of Community Reentry for Women, Male Adolescents, and Their Families and Communities. American Journal of Public Health. 2005;95(10):1725–1736. 104. Metraux S, Culhane DP. Homeless Shelter Use and Reincarceration Following Prison Release: Assessing the Risk. Criminology and Public Policy. 2004;3(2):201–222. 105. Nelson M, Deese P, Allen C. The First Month Out: Post-Incarceration Experiences in New York City. New York: Vera Institute of Justice; 1999. 106. Aidala A, Cross JE, Stall R, Harre D, Sumartojo E. Housing as a Structural Intervention to Reduce Risk Behaviors Among HIV-Positive People. Paper presented at the 2003 CDC Prevention Conference, Atlanta, GA. 2003. 107. Riley ED, Bangsberg DR, Guzman D, Perry S, Moss AR. Antiretroviral Therapy, Hepatitis C Virus, and AIDS Mortality Among San Francisco's Homeless and Marginally Housed. Journal of Acquired Immune Deficiency Syndrome. 2005;38(2):191–195. 108. Moss AR, Hahn JA, Perry S, Charlebois ED, Guzman D, Clark RA, Bangsberg DR. Adherence to Highly Active Antiretroviral Therapy in the Homeless Population in San Francisco: A Prospective Study. Clinical Infectious Diseases. 2004;39(8):1190–1198. 109. National Commission on Correctional Health Care (NCCHC). The Health Status of Soon-to-be-Released Inmates: A Report to Congress. April 2002. Available at: http://www.ncchc.org/stbr/Volume2/ Health% 20Status%20(vol%202).pdf. 110. Zack B. HIV Prevention: Behavioral Interventions in Correctional Settings. In: Greifinger R, ed. Public Health Behind Bars: From Prisons to Communities. New York: Springer; 2007: 156–173. 111. World Health Organization. Prison Health is Public Health. Retrieved on March 12, 2008. Available at: http://www.euro.who.int/features/2005/featurewad/20051119_8. Acknowledgements amfAR is extremely grateful to Barry Zack (formerly of Centerforce) for his general guidance about HIV prevention in correctional settings, and to the following individuals for their helpful comments on an earlier version of this document: Philip Fornaci, D.C. Prisoners’ Project of the Washington Lawyers’ Committee for Civil Rights and Urban Affairs • Peter Gamache, M.B.A., M.L.A., M.P.H. (R.N.), University of South Florida • Deborah M. Golden, Esq., D.C. Prisoners’ Project of the Washington Lawyers’ Committee for Civil Rights and Urban Affairs • Adisa Griffin, Prison Initiative Manager, National Minority AIDS Council • Olga Grinstead, Ph.D., University of California, San Francisco • Kathleen Morrow, Ph.D., Brown University • Josiah Rich, M.D., M.P.H., Brown University • Jackie Walker, ACLU National Prison Project • Milton Zelermeyer, The Legal Aid Society, Prisoners’ Rights Project 11 www.amfar.org Public Policy Office 1150 17th Street NW Suite 406 Washington, DC 20036-4622 Tel: 202-331-8600 Fax: 202-331-8606 Susan J. Blumenthal, M.D., M.P.A. Senior Policy and Medical Advisor Monica S. Ruiz, Ph.D., M.P.H. Acting Director, Public Policy Karine Dubé, M.Phil. Research and Program Analyst Elisha Dunn-Georgiou, J.D., M.S. Legislative Analyst Gay Glading Office Manager New York Office 120 Wall Street, 13th Floor New York, NY 10005-3908 Tel: 212-806-1600 Fax: 212-806-1601

