First Aid for Asthma, Allyn & Bacon, 1996
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
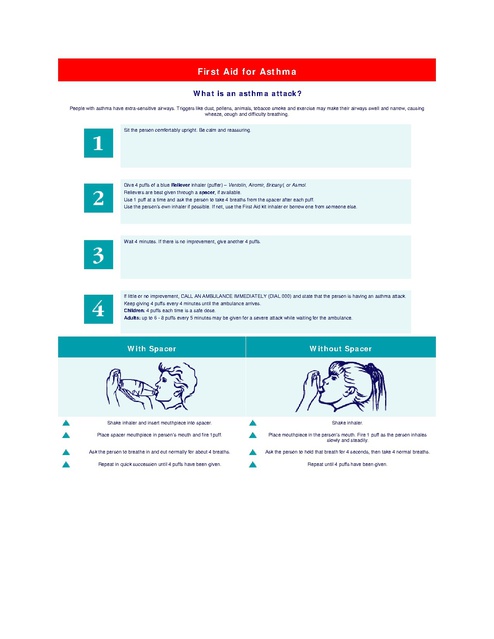
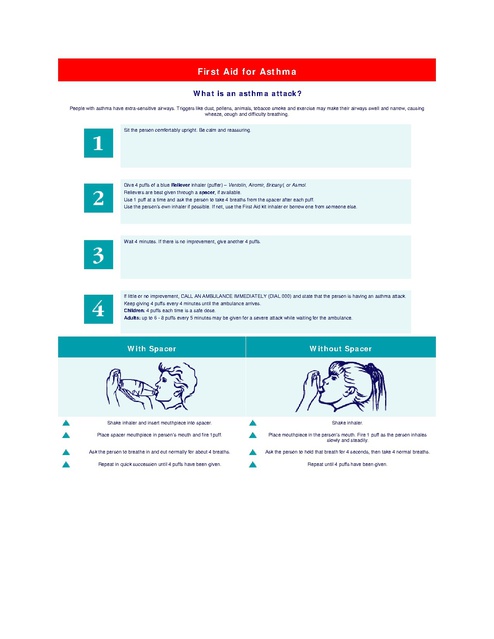
First Aid for Asthma What is an asthma attack? People with asthma have extra-sensitive airways. Triggers like dust, pollens, animals, tobacco smoke and exercise may make their airways swell and narrow, causing wheeze, cough and difficulty breathing. Sit the person comfortably upright. Be calm and reassuring. i-i N Give 4 puffs of a blue Reliever inhaler (puffer) – Ventolin, Airomir, Bricanyl, or Asmol. Relievers are best given through a spacer, if available. Use 1 puff at a time and ask the person to take 4 breaths from the spacer after each puff. Use the person’s own inhaler if possible. If not, use the First Aid kit inhaler or borrow one from someone else. Wait 4 minutes. If there is no improvement, give another 4 puffs. M If little or no improvement, CALL AN AMBULANCE IMMEDIATELY (DIAL 000) and state that the person is having an asthma attack. Keep giving 4 puffs every 4 minutes until the ambulance arrives. Children: 4 puffs each time is a safe dose. Adults: up to 6 - 8 puffs every 5 minutes may be given for a severe attack while waiting for the ambulance. With Spacer Without Spacer Shake inhaler and insert mouthpiece into spacer. Shake inhaler. Place spacer mouthpiece in person’s mouth and fire 1puff. Place mouthpiece in the person’s mouth. Fire 1 puff as the person inhales slowly and steadily. Ask the person to breathe in and out normally for about 4 breaths. Ask the person to hold that breath for 4 seconds, then take 4 normal breaths. Repeat in quick succession until 4 puffs have been given. Repeat until 4 puffs have been given. How to handle an emergency How to recognise a serious asthma attack An asthma attack can take anything from a few minutes to a few days to develop. During an asthma attack coughing, wheezing or breathlessness can quickly worsen. Signs of an acute asthma attack requiring immediate action: • Severe shortness of breath (struggling to breathe) • Rapid shallow breathing • Wheezing sound when breathing in and out (if wheezing stops with no improvement in symptoms it is an extreme EMERGENCY) • Chest tightness (feels as if someone is sitting on chest) • Unable to speak more than one or two words per breath • Distressed or feeling frightened • Little or no improvement after using reliever medication (Bricanyl, Ventolin or Salamol) • Areas at base of throat and between ribs 'sucking in' and out • Blueness around the lips • Hunching over Note: Not all of the above symptoms may be present. During an asthma attack, young children may appear restless, unable to settle and may have problems eating due to shortness of breath. They may also have severe coughing and vomiting. If you (or anyone in your care) have any of the above signs, call an ambulance (dial 111) straight away and follow the 4-Step Asthma Emergency Plan. 4-Step Asthma Emergency Plan 1. Sit the person upright, and loosen any tight clothing. Stay with the person, remain calm and provide a reassuring attitude to help avoid panicking. 2. Without delay give 6 separate puffs of a reliever (Ventolin or Salamol). The medication is best given one puff at a time via a spacer device. Use the puffer on its own if you don't have a spacer. Ask the person to take 4 breaths from the spacer after each puff of medication. 3. Wait 4 to 5 minutes. 4. If there is little or no improvement, repeat steps 2 and 3. If there is still little or no improvement, continuously repeat steps 2 and 3 whilst waiting for the ambulance. EMERGENCY CARE FOR ACUTE ASTHMA ATTACK An asthmatic told me that if you wanted to know how an acute asthma attack felt, put a straw in your mouth and purse your lips around it, then hold your nose while going for a mile run breathing only through the straw. I tried it for a block and got the picture. The acute asthma attack varies in duration, intensity, and frequency and reflects airway obstruction due to: • • • • • • • • • • • • • • Bronchospasm (generalized spasm of the bronchi) Swelling of the mucous membranes in the bronchial walls Plugging of the bronchi by thick mucus secretions. A typical acute attack may feature the following signs and symptoms: Victim sits upright, often leaning forward, fighting to breathe Spasmodic, unproductive cough Whistling, high-pitched wheezing, usually during exhalation Very little movement of air during breathing, even at rest Hyperinflated chest with air trapped in the lungs because of increased Obstruction during exhalation Rapid, shallow respirations Rapid pulse (usually more than 120 beats per minute) Fatigue Use of accessory muscles in the neck and shoulder to aid breathing. EMERGENCY CARE The three goals of emergency care for an acute asthma attack are to improve oxygenation, relieve Bronchospasm, and improve the victim's ventilation. • • • • • • Remove the person from the source of the reaction, or remove the source from them (get them out of the cold air, have them stop exercising, remove them from a polluted environment, etc.). Establish an airway and assist ventilations if necessary (mouth-to-mouth breathing if they aren't breathing). Assist the victim with his/her medication. Shake the inhaler and spray once in the air. Have the victim breathe in and out once then insert the inhaler and assist with three applications of the medication, having them hold each one in the lungs before breathing out. If they don't have their inhaler, antihistamines will do some good. Stay calm and keep the victim as calm as possible; stress, cold and emotional intensity worsen the asthma. Keep the victim in a position of comfort, usually seated. If you do not anticipate aspiration, give the victim as much warm fluid by mouth as possible to aid with the mucus. Call 911 if the condition persists or worsens. First Aid For Colleges and Universities, 6th Edition, By Hafen and Hafen, Allyn & Bacon, 1996 pp.28789) An acute asthma attack is a frightening experience for both the patient and any onlookers. Imagine being suddenly unable to breathe -- most people would react with sheer panic. If you know these asthma attack treatment basics, you'll be far better equipped to help anyone having such an emergency. And these situations are not rare at all. You might be at a restaurant having lunch with a few friends and one of them suddenly gasps for breath and seems to panic. The problem is even worse if it involves small children; they just can't grasp what's happening to them. Asthma emergency treatment know-how can be a definite help in these situations. Here are several things you need to be aware of. * Remember that when someone is having an attack, they'll almost always find it easier to breathe while sitting up than lying down. So don't make the mistake of getting them to lie down -- settle them into a sitting position and make them as comfortable as possible. * In most cases, the patient already knows exactly what needs to be done to help her, because this is probably not the first attack she's facing. If she is in a position to talk (and she may not be), just ask her what you should do. She may well be carrying an inhaler, so ask if she has one and where it is kept. Also ask if she wants you to call for help. Many patients carry written instruction cards with an asthma attack treatment plan. If she can't talk, look for such a card. Follow the instructions. * Here's the single most important asthma treatment protocol -- help her use the inhaler. There is nothing you can do that will have the same effectiveness as getting the patient to use an inhaler. What is an inhaler? Basically, it's a device designed to deliver specific doses of medication. Medication that relaxes the patient's air passages thus bringing breathing back to normal. In fact, an inhaler is so critically important that doctors say if the patient doesn't have one with her, use someone else's to reduce the breathing problem. How do you use an inhaler? Get the patient to take two to four puffs immediately (unless she tells you something else, or her instruction card does). Then wait for around five minutes before giving the next dose. Hold the mouthpiece of the inhaler between her lips. Tell him before you give a puff so that she can inhale at the same time. After giving one puff, wait a few seconds before you give another one. Wait till you think she is ready for another puff or she indicates that she is. Using a spacer can allow her to breathe in the medication over several breaths, instead of in just one breath. A spacer positioned between the inhaler and the patient's mouth can hold in the medicine between breaths. You can improvise a simple spacer by rolling up paper and creating a short tube. * After giving medication, continue to observe the patient closely for a few minutes. Is there a distinct improvement in her condition, is she getting any relief? Is her breathing easier than before? * If you think the medication is not having an effect on her within say 10 minutes, it is best to get help. Call an ambulance. In the meanwhile, continue to give her medication -around four puffs every five minutes. Even if it appears that the medication is not helping, it can prevent her attack from getting worse. * As the person taking care of the patient, your demeanor counts. If you panic, it can actually make her attack worse, because she will feel it is out of control and respond accordingly. So stay calm and talk to her in a calm manner. This is critical. Keep these asthma attack treatment essentials in mind. You will be far better prepared to deal with emergency situations and possibly even save a life by bringing an attack under control.

